Nick Mitrousis and Sri Ray-Chauduri, Technology & Engineering editors
Cancer. For most of us, that word conjures up memories of a friend or family member who succumbed to the disease. Despite decades of scientific work and billions of dollars spent developing new treatments, cancer remains a leading cause of death worldwide. So it’s no surprise that the emerging idea of immunotherapy has created immense excitement among researchers and patients. Could this be the silver bullet we’ve been searching for?
Although many of us have only heard of immunotherapy recently because of successful clinical trials on blood cancers, the concept is more than 100 years old. In 1909, Paul Ehrlich first hypothesized that cancer would be much more prevalent if it were not for our immune system [1]. He pictured cancer as a regular pathogen. Our immune system is uniquely adept at identifying and eliminating bacteria, fungi, or viruses because they differ from our regular cells. And the thing is, cancer cells are different too. Due to genetic alterations, they express proteins or markers that are not as commonly found in the rest of our body. Perhaps, Ehrlich figured, the immune system identifies these aberrant proteins and eliminates the cells that contain them.
Many medical breakthroughs are surrounded by huge hype, but the results being produced by immunotherapy seem to be the real deal.
It took more than 50 years and significant advances in our understanding of immunology for Paul Ehrlich’s theory to re-emerge. The current view among cancer immunologists is that although the immune system is capable of attacking tumors, those tumors are great at playing hide and seek. Tumors can escape detection by concealing the surface molecules, called markers, which the immune system uses to identify them. Others produce substances that suppress immune response. Immunotherapy focuses on tweaking the interactions between tumors and the immune system to overcome these defenses.
Some of the most impressive data come from early phase clinical trials for blood cancers, specifically B-cell leukemias. Patients that had relapsed or were unresponsive to chemotherapy received genetically modified T-cells, which are the immune system’s “killer” cells. The T-cells were tailored to target CD19, a protein that is present on the surface of all B-cells. This means that the modified T-cells (commonly called CAR-T cells (i.e. Chimeric Antigen Receptor-modified T cells)) bind to any cell carrying CD19 and kill it. Of patients that initially had only a few months to live, complete remission was achieved in up to 90% of cases. At least one patient has remained tumor free for five years. Despite some serious side effects, such as the elimination of normal B-cells along with the cancerous ones, the striking results marked a huge leap forward for the field of immunotherapy.
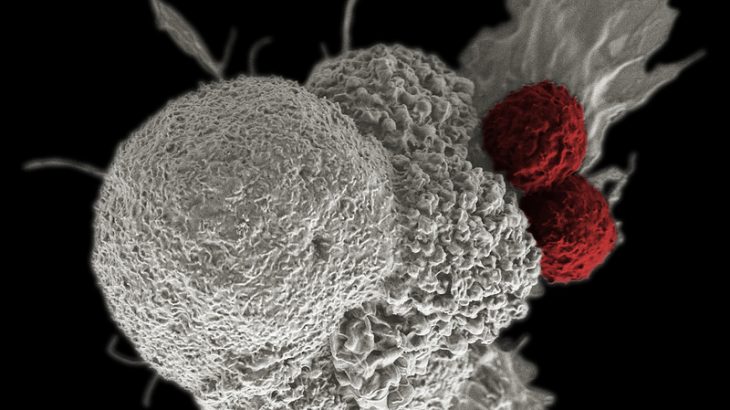
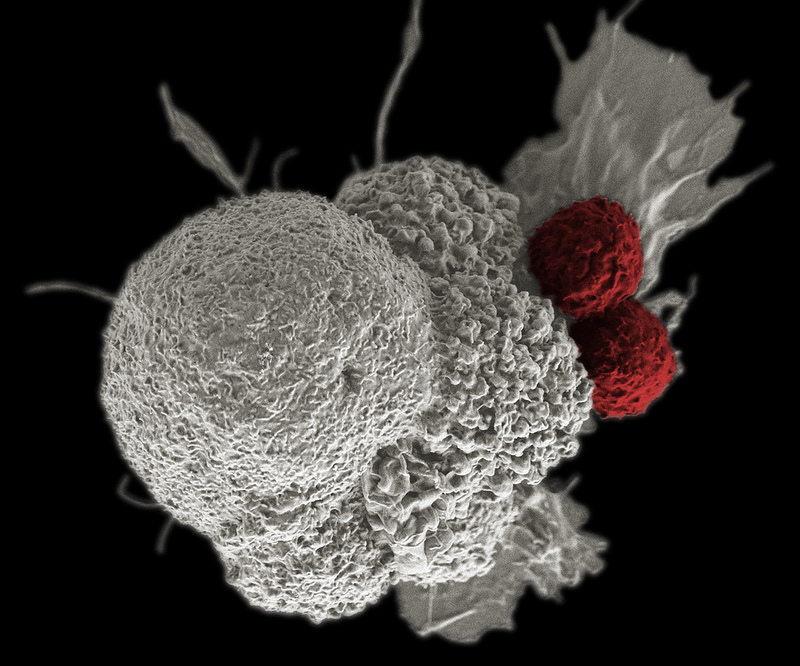
Pseudo-colored scanning electron micrograph of an oral squamous cancer cell (white) being attacked by two cytotoxic T cells (red), part of a natural immune response (Credit: NIH Image Gallery CC by 2.0)
While the remarkable success of such immunotherapy approaches in leukemia cases is encouraging, these treatments have been less effective in solid tumors. Successfully applying CAR-T cell approaches in different cancer types is the next frontier in immunotherapy. Certain cancers (such as B-cell leukemia) may be more amenable to CAR-T-cell therapy because completely eliminating all B-cells is not fatal if the patient receives appropriate treatment. This simplifies the process of selecting a marker on which to target the T-cells. Also, CAR-T-cells may have an easier time tracking and eliminating cancer cells in a liquid such as blood, where they do not need to penetrate into a solid tumor and overcome inhibitory molecules present in its microenvironment. Researchers are currently studying the intricacies of the tumor microenvironment to identify new ways of increasing the success of CAR-T approaches for solid tumors.
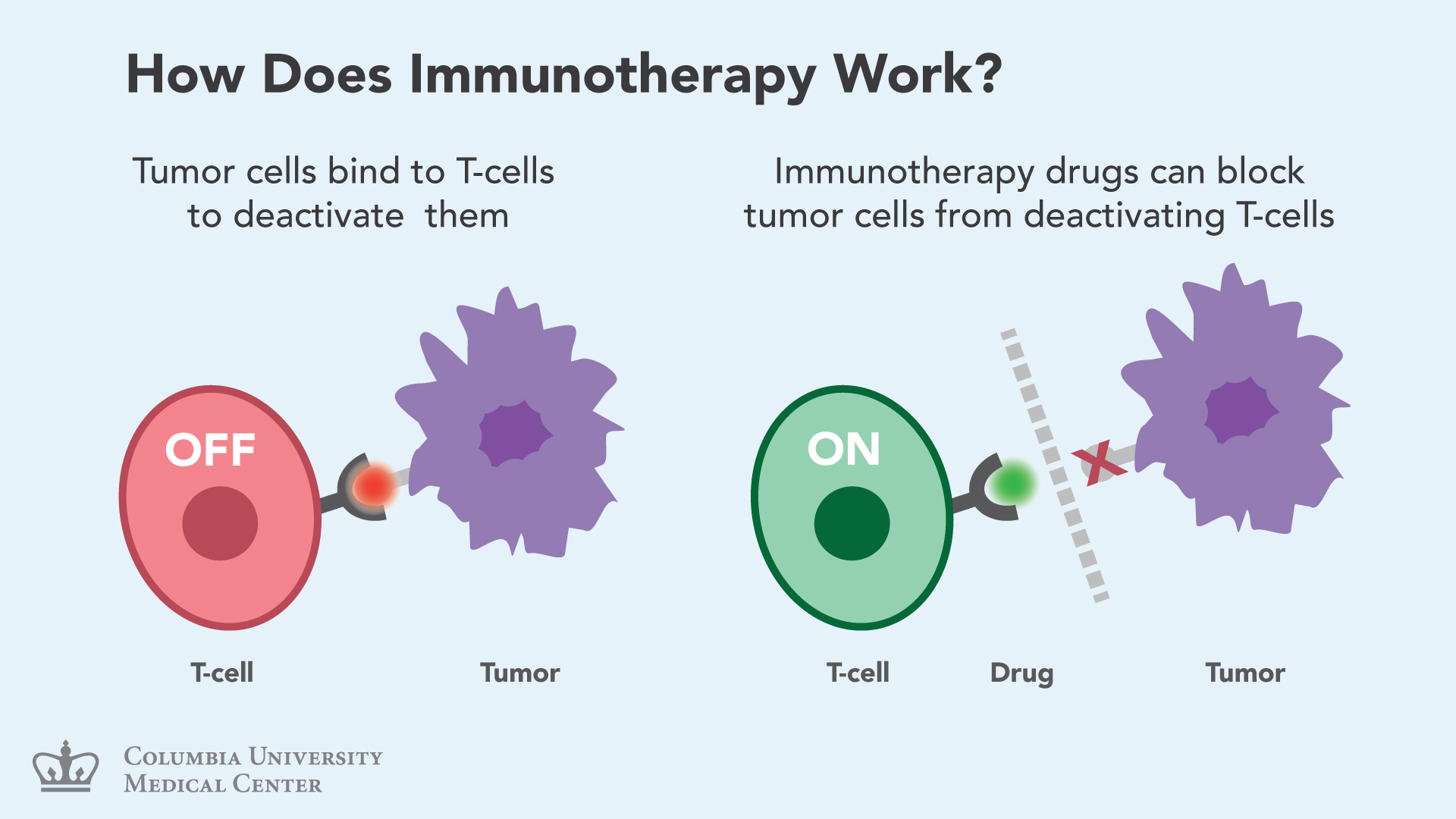
But immunotherapy’s toolkit includes other approaches besides CAR-T-cells. For example, the “checkpoint blockade” earned Texas researcher James Allison Canada’s top medical prize, the Gairdner award, last October. Checkpoint blockade therapies use inhibitors targeting molecules that are natural brakes for the immune system. Releasing these brakes bolsters the activity of the immune system, which then has a better chance of overcoming the suppressive environment of tumors. Such therapies have shown astonishing results in melanoma, and are currently in clinical trials for many other cancers.
Cancer cells can bind to T-cells and “turn-off” their ability to detect and kill tumor cells. Immunotherapy drugs bind to T-cells and keep them “on” by blocking a tumor cell’s access to the T-cell. Read more about Immunotherapy at the Columbia University Medical Center. (Credit: Columbia University Medical Center – used with permission)
Immunotherapy appears to be where the field of cancer treatment is headed. Though still in its clinical infancy, immunotherapy has demonstrated an unprecedented potential for successfully treating certain tumor types. Combination therapies, where traditional chemotherapy is used along with immunotherapy or different types of immunotherapy are applied together, are becoming increasingly popular.
Currently most of these approaches are only available to patients through clinical trials. A more thorough understanding of why certain treatments only work with specific cancer types could expand this small repertoire to more cancers, and follow-up clinical trials would then assess the safety and efficacy of these novel treatments in real patients. Exactly how these therapies, which often come at prohibitive costs, will be incorporated into the healthcare system and made available to all patients remains to be seen.
Earlier this year, Silicon Valley investor Sean Parker made headlines when he announced a $250 million grant to advance development of immune therapies for treating cancer by creating a consortium of 40 different labs in six different institutions. Although such initiatives are necessary to turn the promise of immunotherapy into reality, Canada is still working to create such large scale endeavors. Currently, The Princess Margaret Cancer Foundation’s Tumour Immunotherapy Program in Toronto is the primary comprehensive immunotherapy center in the country.
Many medical breakthroughs are surrounded by huge hype, but the results being produced by immunotherapy seem to be the real deal. The ultimate success of immunotherapy may lie in its ability to combine scientific and engineering efforts and unite research goals. The ultimate success of immunotherapy may lie in its ability to combine scientific and engineering efforts and unite research goals.
References
- Ehrlich, P. Ueber den jetzigen stand der Karzinomforschung.Ned. Tijdschr. Geneeskd.5, 273−290 (1909).