By Qiaochu Liang, Biology & Life Sciences co-editor
Although COVID-related restrictions have eased and the social activities of Canadians have resumed, the pandemic persists, especially with the emergence of SARS-CoV-2 variants. As information gathered from individual testing has decreased, Canadian health authorities have adopted a more effective approach for keeping track of the presence and trends of the virus.
Since 2020, wastewater has become an important resource for detecting the presence of SARS-CoV-2 across Canada. Today, Canada has a strong, nationwide wastewater surveillance system with standardized protocols.
Why wastewater?
The traditional COVID surveillance system relies on individual testing and recorded COVID-19–related hospitalizations. But these measures depend on the availability of resources and miss mild or asymptomatic cases. Because public health agencies require more real-time and accurate data to support evidence-based decision-making, an early detection method for the presence of COVID was needed. Researchers in the Netherlands were the first to find that SARS-CoV-2 RNA is detectable in patients’ feces and in a community’s wastewater. They showed that the viral signal was detected in wastewater at least six days before the first case was reported through the traditional surveillance system. Since then, over 50 countries, including Canada, have adopted SARS-CoV-2 wastewater monitoring.
Wastewater surveillance is an efficient approach for determining the prevalence of COVID because it samples the whole population rather than a few individuals. That means wastewater analysis does not identify who has COVID-19, but rather monitors the virus’ circulation within the community. While massive-scale individual testing is complicated and expensive to undertake, wastewater surveillance is independent of healthcare access or testing capacity. Furthermore, because both symptomatic and asymptomatic individuals shed SARS-CoV-2 in their feces, wastewater analysis delivers more accurate data about the prevalence of the virus than individual testing, producing a better understanding of the course of the pandemic.
Infected individuals can take up to 14 days to develop symptoms, or they can remain asymptomatic. Either way, they start shedding the virus in their urine or feces soon after becoming infected (5-6 days before the first symptoms). This means that wastewater analysis also serves as an early warning system that creates a window of opportunity for health authorities to take quick action to get ahead of an outbreak.
How does wastewater surveillance work?
The procedures for regular SARS-CoV-2 screening in wastewater are based on work done to monitor other pathogens. Prior to the emergence of COVID-19, wastewater-based epidemiology was used to identify and quantify pathogens such as norovirus and hepatitis A.
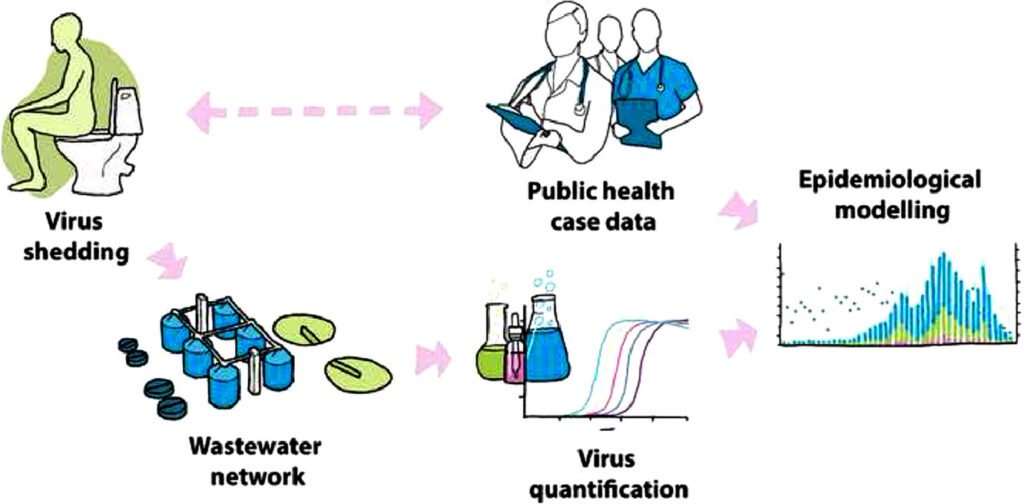
The process of wastewater surveillance includes collecting samples at wastewater treatment plants, isolating the virus, detecting the genetic material of SARS-CoV-2 (RNA), and quantifying the viral load. A nationwide wastewater surveillance network that covers over two thirds of the population of Canada was established (see the Map of Pan-Canadian Wastewater Network). Wastewater is collected three times a week from the wastewater catchment that flows into a treatment plant. Samples are transported to public health laboratories where the virus fragments in each sample are concentrated by filtration for molecular analyses. The viral RNA is extracted and quantified with PCR-based approaches. The highly sensitive sequencing technology identifies all of the circulating variants in the wastewater. This information reveals which variants are dominant and can provide valuable insights into emerging virus mutations.
Steps used in wastewater surveillance for COVID-19. The final step (not shown) is the communication of the wastewater analysis to the community. Image: Polo et al. (2020), CC BY 4.0.
Major hurdles for this process are transportation delays and population coverage. The Government of Canada is working to overcome these barriers by increasing the reach of monitoring through enhanced local testing and more wastewater sampling sites. To make the data as reliable as possible in different settings, scientists are constantly refining techniques for sample collection and analysis.
How is wastewater data shared and used?
A screenshot of the wastewater data in my community (Vancouver) shows the viral load detected in wastewater and how it changes over time. Image: BC Centre for Disease Control.Once wastewater samples have been analyzed, the results are sent to epidemiologists and data analytics partners for review and summation. The epidemiologists track the viral load in the wastewater over time, while medical geographers map the data to specific water catchments. Overlaying the incidence of community cases with wastewater data reveals a correlation between the viral signal detected in wastewater and case counts — a surge in COVID-19 cases correlates with a spike in the wastewater viral load. Wastewater data are also combined with other data, such as geographical context (for example, areas with high tourism or neighbouring communities with a high number of cases), to pinpoint hot spots and identify the causes of spikes in infections. The epidemiologists also use the data to build predictive models to forecast the infection trend.
The resulting reports are disseminated to health departments, including medical health officers and epidemiologists at regional health authorities. Wastewater analysis is playing a big role in shaping policy because it helps health authorities evaluate the effectiveness of measures to control the spread of COVID-19. An effective measure, such as reintroducing restrictions, should be followed by a decrease in the viral signal in wastewater, which further informs the officials’ decision-making.
Wastewater analysis results are also available to the public through an online dashboard that tracks the SARS-CoV-2 viral load in wastewater in major communities across Canada. Individuals can select the region where they live to access the wastewater signals in their area, assess the risks of infection, and make informed decisions about their personal risk management measures.
A screenshot of the wastewater data in my community (Vancouver) shows the viral load detected in wastewater and how it changes over time. Image: BC Centre for Disease Control.
Ongoing and future applications of wastewater surveillance
Wastewater surveillance is not limited to community-based testing. Samples can be collected from specific areas of interest to provide more focused information. For instance, wastewater testing has been implemented on planes arriving from other countries to help scientists track existing and emerging pathogens. Sewage collection from airplanes, school dormitories, or long-term care homes offers more specific insights into sources of infection.
Wastewater surveillance can also be used for the rapid assessment of emerging threats; this helps with preparedness for future pandemics. Wastewater sampling is currently being used to monitor Mpox, influenza, RSV and many other respiratory viruses, and to screen for antimicrobial-resistant organisms.
Wastewater sampling is a powerful tool for assessing the presence and prevalence of a variety of infectious diseases. According to the Honourable Jean-Yves Duclos, Canadian Minister of Health: “Wastewater monitoring is the future of public health surveillance for infectious diseases in Canada. It is an innovative tool that currently assists in determining the levels of COVID-19 in communities and provides an early warning to public health authorities of COVID-19 variants.” However, wastewater surveillance will not replace data from individual testing, reported hospitalizations, and deaths, because no single indicator can give a full picture of the COVID-19 pandemic.
Feature image: Testing wastewater provides valuable information about the presence and spread of COVID-19 in Canada. Image: aleksandarlittlewolf on Freepik.