by Emerson Gaglardi, New Science Communicator
In 2016, 36.7 million people around the world were living with HIV (human immunodeficiency virus) infections. To put this in perspective, that is about the same as the current population of Canada.
Without treatment, HIV dramatically reduces the number of infection-fighting white blood cells over a period of about 10 years, destroying the immune system of the infected individual. The destructive activity of HIV leads to a condition called AIDS (acquired immune deficiency syndrome), which makes people more susceptible to a variety of infections and diseases.
Worldwide, 35 million people have died from AIDS-related illnesses since the beginning of the AIDS epidemic in 1981.
Unfortunately, the general public generated a significant amount of fear and hysteria surrounding HIV/AIDS because of misunderstandings about HIV, who it can infect, and how it spreads. As a result, people living with HIV have been stigmatized since the beginning of the AIDS epidemic.
These attitudes are a major barrier to the development of effective HIV prevention and treatment efforts, as well as access to these programs by individuals who are vulnerable to infection.
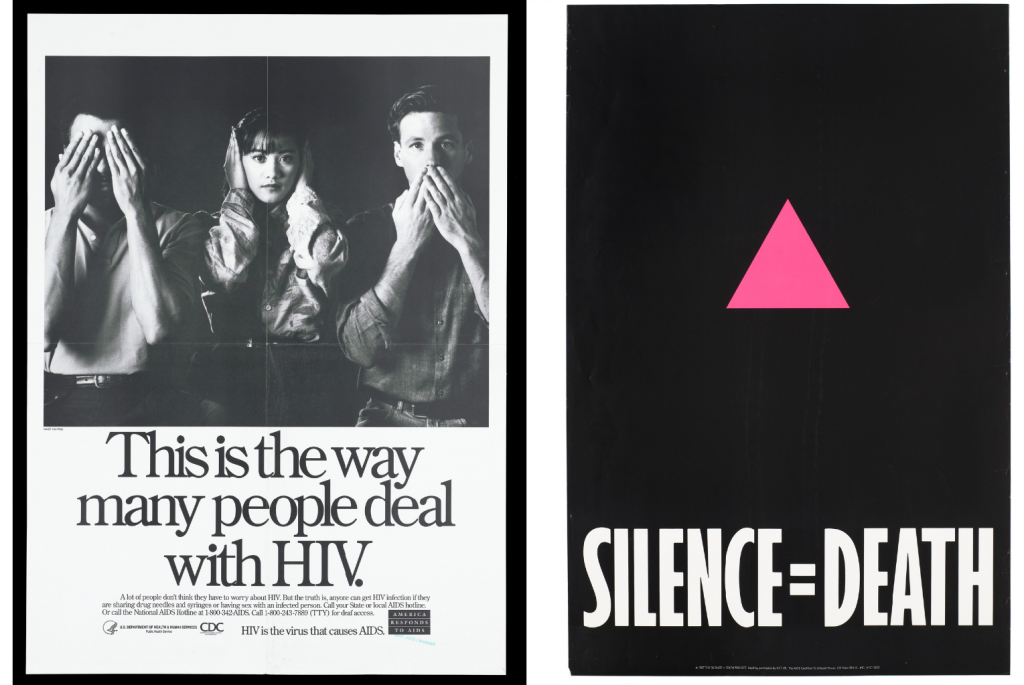
The belief that HIV only affected gay men, drug users, or sex workers resulted in a large proportion of the general public choosing to remain ignorant about the virus, as indicated in this poster made by the US Center for Disease Control (image via Wellcome Collection, CC BY-NC). Organizations like ACT UP have also campaigned to increase awareness of HIV/AIDS by encouraging open dialogue about the issue (image via Wellcome Collection, CC BY-NC).
Fortunately, increased understanding of HIV has counteracted this fear and stigma, and has allowed for the development of effective treatments. For example, over half of people living with HIV currently have access to antiretroviral medications, which have been proven to dramatically extend the life of HIV-positive individuals.
However, while these medications are highly successful and allow people living with HIV to lead normal lives, history has shown that vaccines are the most effective way to eradicate infectious diseases.
Scientists around the world, including Ralph Pantophlet at Simon Fraser University, are hard at work to develop an effective HIV vaccine. This task is proving to be incredibly difficult.
Vaccines teach the immune system to respond to particular viruses by exposing the immune system to components of those viruses. For example, seasonal influenza vaccines expose the immune system to components of the membrane that surrounds the influenza virus. This teaches the immune system to recognize those components during an influenza infection and quickly begin producing antibodies that bind to those same components, neutralizing the virus and stopping it from causing illness.
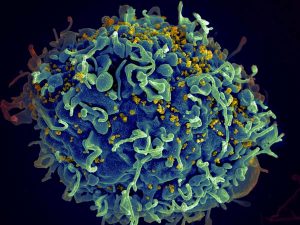
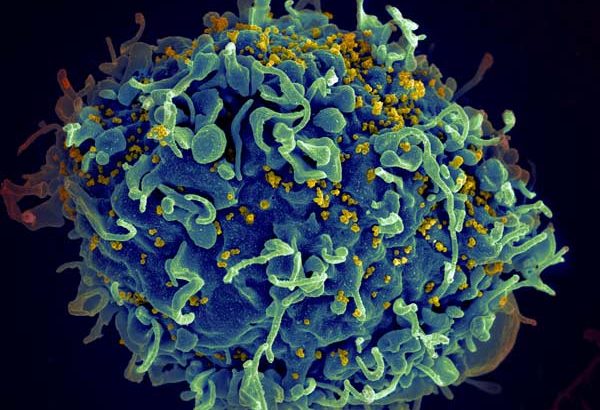
HIV infecting a human cell. Photo: Seth Pincus, Elizabeth Fischer, and Austin Athman, National Institute of Allergy & Infectious Diseases, National Institutes of Health
If vaccines work for viruses like influenza, why is it so difficult to develop a vaccine for HIV?
For any virus to spread throughout an infected individual, it has to replicate itself. HIV is no exception. However, since the enzyme that carries out HIV replication is particularly error-prone, it is highly likely that HIV will mutate during replication. These rapid genetic changes result in a wide variety of HIV offspring.
“The genetic variation of HIV in a single infected individual is about the same as the yearly genetic variation that you would see in influenza virus globally,” says Pantophlet. “As HIV replicates, the composition of the [components of the HIV membrane] changes at a much higher rate than, for example, components of the influenza virus membrane.”
With HIV changing so rapidly, it is challenging to identify a component of the virus after which to model a vaccine. Essentially, an HIV vaccine would have to mimic a component of HIV that does not change between different HIV offspring. This component could then be introduced into humans to teach the immune system to recognize and attack HIV. Fortunately, Pantophlet and his team of researchers seem to have identified a component of the HIV membrane that may do the trick.
“By studying many different HIV-infected individuals, we’ve identifed [regions on the HIV membrane that do not vary a lot]. In the lab, you can then design a molecule that presents this site to the immune system and prepares the immune system to respond when ‘real’ HIV comes along.”
Pantophlet’s research group has “[designed] a sugar molecule that looks like what you would find on the surface of HIV, … so that when animals – and eventually humans – are immunized with this molecule, there [is] an ensuing immune response … that will allow the immune system to recognize HIV in the case of an infection.” Indeed, this “designer” molecule results in an immune response against HIV when injected into animal models.
Extensive research and clinical testing are still needed to determine the effectiveness and safety of using this molecule as an HIV vaccine for humans. Nonetheless, this innovative and exciting research at Simon Fraser University shows that advancements are being made in the challenging field of HIV vaccine development, bringing us closer to the eventual eradication of HIV/AIDS worldwide.
~30~




Thanks! I’m glad progress is being made in the eventual eradication of HIV/AIDS worldwide.
~Carla
Great article, Emerson. Amazing progress in the quest for the eradication of HIV/AIDS worldwide.