Zahra Nasser and Nada Salem, Chemistry editors
People with diabetes have measured their blood sugar the same way since the 1970s – a painful daily prick of the finger. While most have no choice but to get used to this, it shouldn’t have to be that way. Monitoring technology has come a long way over the last 40 years. If you want to start monitoring your heart rate, blood oxygen levels, or sleeping patterns, all you need is a trendy Fitbit watch on your wrist. So when will medically necessary monitors finally start catching up to innovations in monitoring technology?
People with diabetes cannot properly regulate their body’s sugar levels, specifically glucose. Normally, a hormone called insulin helps regulate the amount of glucose in the blood. When blood sugar levels are high, such as after a meal, insulin ensures our cells absorb glucose, providing them with a source of energy to use or store for later. Type II diabetes is the most common type of this disease. It develops when cells become less responsive to insulin (insulin resistant). Type I diabetes occurs when the body fails to make enough insulin or none at all. If left untreated, both types of diabetes cause blood sugar levels to skyrocket, eventually leading to nerve and organ damage.
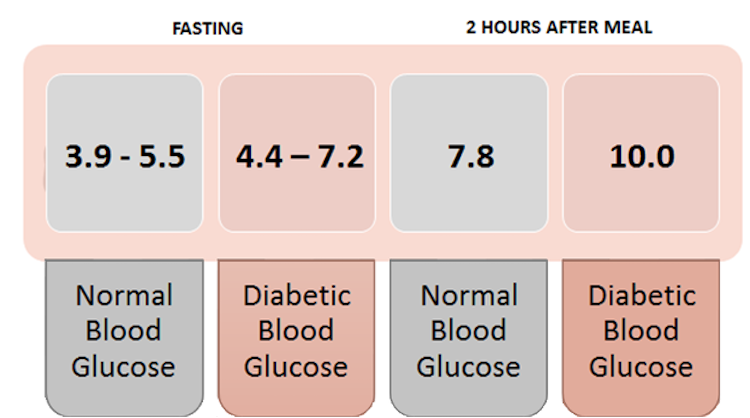
Blood glucose monitors measure blood sugar in units of millimoles per litre (mmol/L). Even minor elevations in blood sugar can be harmful when left untreated. Image by author based on data from the American Diabetes Association
Diabetic patients need to measure their blood sugar levels daily to monitor and manage their health. The majority do so with a sharp finger prick to draw a drop of blood onto a test strip. The process is “time-consuming and inconvenient,” says Amanda Stercyzk, Manager of Research and Public Policy at Diabetes Canada. Newer methods such as real-time or intermittently-scanned continuous glucose monitors (rtCGMs and isCGMs, respectively) reduce the difficulty of glucose monitoring. These technologies use a temporary sensor, worn for 6-14 days, that automatically measures glucose levels every few minutes or when scanned. These diagnostic tools still rely on a blood sample, making them invasive. The uncomfortable finger prick method is still more accurate than continuous blood monitoring and is often the recommended option. However, painless and precise measuring tools may be just around the corner.
While researching non-invasive methods to measure glucose, researchers at the University of Waterloo discovered that the solution could be right under our noses: saliva! Saliva is produced and secreted by the salivary glands and contains a broad array of molecules. Wenyu Gao, a Ph.D. student, led a study that developed a prototype sensor that measures glucose levels in saliva.
The diagnostic process breaks down the saliva sample into its many components. The sensor contains a graphene sheet with copper nanomaterials, specifically Cu2O nanocubes. This composition of materials enables a specific reaction between copper and glucose. Copper is a transition metal; it can carry different charges by either gaining or losing electrons. When copper is oxidized (by removing electrons), the positively charged copper can catalyze the reaction that creates gluconic acid from glucose. This reaction causes a current to pass through the sensor’s electrode; a higher level of glucose results in a higher electric signal.
Why would we measure salivary sugar when diabetic people are concerned about blood sugar? It turns out, blood and saliva carry similar information. There’s a constant exchange of materials between our bloodstream and saliva, which means saliva often contains the same biomarkers we look for in blood to monitor or diagnose a disease. Gluconic acid measured from saliva is a reliable proxy for a blood sugar measurement – no blood or needles required.
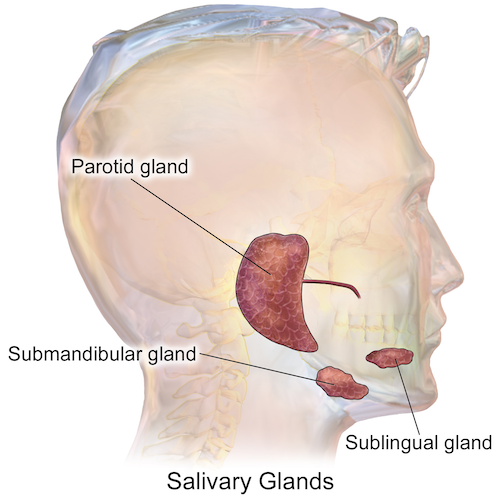
The parotid gland contains saliva with the highest glucose concentration. It also shows the strongest correlation to blood sugar among the three salivary glands. Image by Blausen.com staff (2014) in Medical gallery of Blausen Medical 2014. WikiJournal of Medicine, CC BY 4.0
While we’ve historically relied on blood to give us information on our health, saliva tells a parallel story about what’s happening in our bodies. In 2015, research conducted at University of California, Los Angeles provided ground-breaking evidence of the potential of saliva testing. It showed that some types of ribonucleic acid (RNA) found in human cells are also present in saliva, a surprising finding since saliva contains enzymes that can degrade RNA. The RNAs are cellular messengers that are also found in the bloodstream and can be used as biomarkers for certain diseases. They leak out into the gums or salivary glands, thereby allowing direct exchange of molecules between saliva and the bloodstream. This discovery initiated a conversation about the validity and accuracy of saliva as the medical diagnostic tool.
“Saliva is one of the body fluids [that] reflects the condition of human health,” says Gao. “[It] contains biomarkers of different diseases, and the concentration of biomarkers will increase with the severity of the disease.”
The need for a non-invasive diagnostic for diabetes is secondary to accurate measurements. For Type 1 diabetic patients, who don’t produce insulin, information about how certain activities or the time of day affect their glucose level is critical for understanding their health and appropriate treatment. For saliva testing to become a mainstay of glucose monitoring, it must be both accurate and easy to do.
A study published in 2014 directly comparing salivary glucose with blood glucose revealed that saliva can differentiate non-diabetic from diabetic patients with an accuracy of 94.2 per cent. Diabetic patients were also differentiated from prediabetic people with 76 per cent accuracy. The technology continues to improve, and Gao is confident in the saliva sensor’s ability to “achieve high sensitivity and selectivity for different biomarkers with advanced technology and materials.”
Saliva glucose monitoring still has to prove itself as an alternative to traditional testing, but the vast potential of saliva is catching the attention of medical researchers beyond the diabetic community. Thanks to advances in nanosensing, the future of saliva as a diagnostic tool looks promising. The Human Salivary Proteome Project, founded in 2005, keeps records of all the proteins present in saliva. We now know that the genetic material used to scan for certain tumours can be found in saliva, making it the method of choice for the early detection of some types of cancer.
So, the next time you go to the doctor, be sure to keep your mouth moist. Your saliva may be the newest roadmap to your health.
~30~





Thanks for sharing informative content.